Diversity in medical education: why it’s crucial to pay attention to gender and ethnicity
-
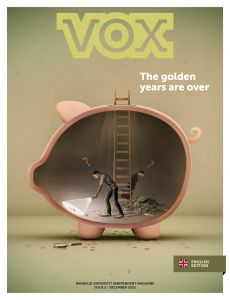
 Illustration: Ivana Smudja.
Illustration: Ivana Smudja.
Radboud University is attempting to diversify its various medical education programmes, not just in terms of student populations, but in lecture material as well. But what are the medical differences between groups that have so far slipped between the cracks?
Themes of diversity and inclusivity are more prevalent than ever at university. One example is professor Karen Stegers-Jager’s recent appointment to make the medical faculty more inclusive and more diverse. Additionally, strategic advisor Geert van den Brink recently called on medical students to participate in the learning network Diversity, Inclusivity, and Equal Opportunities.
And yet, diversity in medical science is not a new topic. In 2021, medical students called for more attention to darker skin tones in dermatology. But there is plenty more ground to gain. What medical differences receive too little attention, according to the experts?
1. Sex
Angela Maas, a retired cardiologist from Radboudumc, is a pioneer when it comes to gender-sensitive medicine. Her career predominately focused on the differences between male and female hearts. These can vary wildly in their behaviour, Maas explains. ‘With heart issues, men tend to get sudden chest pains, while women usually have issues over longer periods of time, such as shortness of breath, exhaustion, sleeping difficulties, or vertigo.’
But the rest of the female body also operates differently than its male counterpart. First of all, there are the visible differences, such as distinctions in body length, weight, muscle density, and fat ratio. Often, the female body also requires lower doses of medicine compared to males, due to differences in the way those medicines are processed by the body. Finally, there’s a host of conditions that have to do with female hormones, such as a heightened risk of blood clots when pregnant or on birth control.
‘The reference man is Caucasian, roughly 1.75 meters tall, and weighs about 80 kilograms’
But despite those differences, medicine often takes males as a baseline, according to Maas. The reference man is Caucasian, roughly 1.75 meters tall, and weighs about 80 kilograms. Anyone who differs from that scheme is considered a variant – women included. And that’s a problem.
According to a study by Voices for Women, 80 per cent of all patients with unexplained health issues are women. Additionally, women are more often diagnosed with psychological issues, such as depression or anxiety. This confirms research by Aranka Ballering, a PhD candidate from Groningen: when men and women see their doctors with the same complaints, women are less likely to be referred to a specialist.
The reason for this, according to Maas, is that the female body used to be subject to the so-called ‘bikini-vision’: the notion that male and female bodies worked the same in every way, save for matters involving genitalia. ‘That notion is completely backwards, but very tenacious.
2. Ethnicity
The ‘average patient model’ in medicine tends to be male. A Caucasian male to be precise. Medical symptoms specific to darker skin tones or people with a migrant background are still underrepresented in education. Colette van Hees, dermatologist at the Erasmus MC, hopes to change that.
Van Hees: ‘The higher the skin’s pigmentation, the harder it is to make out reddened areas. The skin doesn’t turn red, it turns darker. That is why skin conditions such as eczema or psoriasis are recognised less often in people with darker skin tones. That can lead to a misdiagnosis or an underestimation of the condition’s severity.’ This in turn means that those patients suffer from itching, pain, and uncertainty far longer than necessary, according to Van Hees.

That is unfortunate in and of itself, but it can lead to much more serious consequences when doctors overlook acute infections or melanomas. ‘Campaigns aimed at the general population mainly show melanomas on the arms, legs, and torso. But in people with darker skin, melanomas are usually concentrated on the hands, feet, and under the nails. This, combined with the relative rarity of melanomas, means that neither patients nor doctors are properly trained to recognise them.’
The same is true for other conditions linked to ethnicity. For example, Dutch healthcare providers are lacking in knowledge concerning genetic health differences, according to the ‘Migrants, prevention, and healthcare’ report by the national expertise centre for health differences, Pharos.
The report shows that ‘people with sub-tropical backgrounds are more likely to be affected by sickle cell disease and liver cancer’. The authors go on to mention that ‘Hindus are remarkably more likely to develop diabetes’. Other findings include that antidepressants are barely effective in people of Turkish heritage, or that one in three Ethiopians don’t respond to the most broadly used antipsychotic.
Fortunately, the gap in knowledge is slowly closing, says Van Hees. ‘Especially in large cities with major populations of people with a migrant background.’ But, Maas continues, ‘If you really want to make a difference, that knowledge needs to become a part of education. It’s very necessary, but not yet the case in a lot of areas.
3. Gender
The fact that knowledge won’t make a difference until it’s applied to educational programmes is also true for gender-specific issues, according to Sabine Oertelt-Prigione, an internist at Radboudumc. In her job, she mainly deals with so-called ‘sex- and gender-sensitive medicine.’
‘A lot of people think that “gender” refers to your self-identification, but it’s much more than that.’ Oertelt-Prigione refers to issues such as power dynamics based on gender, or societal expectations. ‘Those expectations impact your behaviour, which in turn impacts your health.’
‘The fact that diagnoses are more difficult in certain groups should not be an excuse for lower quality care’
This proves a study on the quality of life in Parkinson’s patients, a condition where specific brain cells slowly atrophy, leading to different behaviours and movement patterns over time. Parkinson’s patients who acted stereotypically male or female before their illness – regardless of sex or gender – turned out to have much more difficulty in organising their lives post-diagnosis.
Oertelt-Prigione: ‘We suspect that this is due to prevailing gender norms. For instance: the men in the study were troubled by the fact that they could no longer be the provider, while the women found it difficult that they couldn’t take care of people the way they used to. Patients with less stereotypically gendered behaviour were much less affected.’
Even so, the role that gender plays remains difficult to study, Oertelt-Prigione admits, because it is so dependant on environmental factors. But for the internist, that is no reason not to study it. Dermatologist Van Hees wholeheartedly agrees. ‘The fact that diagnoses are more difficult in certain groups should not be an excuse for lower quality care.’
Translated by Jasper Pesch