Medicine students organise their own lifestyle course due to dissatisfaction over degree programme
-
 Students Femke de Schutter (20) and Meike Kappen (22) want to see more focus on nutrition and lifestyle in Medicine. Photo: David van Haren
Students Femke de Schutter (20) and Meike Kappen (22) want to see more focus on nutrition and lifestyle in Medicine. Photo: David van Haren
A greater focus on healthy eating and physical exercise in the Medicine degree programme: that's what Nijmegen students of the Student & Lifestyle organisation want to see. To achieve that, they've set up their own course outside the degree programme, and with success.
About fifty years ago, people lived healthily in general. There were few cases of being overweight and if you visited the doctor, you were genuinely ill. Doctors had two possible ways of intervening: medication or surgery.
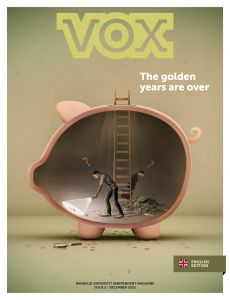
Society progressed and brought us fast food restaurants, colour television and recliners. Since then, people have been exercising less, eating more unhealthily and sleeping worse, with a steep rise in diseases of affluence such as obesity, Type 2 diabetes and cardiovascular diseases. This trend is expected to continue: the RIVM believes that in 2040, 62% of the Dutch population will be overweight (this is currently 49%).
Various Medicine degree programmes are responding to this but only marginally. This to the frustration of a small group of Medicine students in Rotterdam, who felt that there should be a greater focus on the prevention of diseases of affluence. That’s why they set up the Student & Lifestyle Foundation in 2016. There has been a Nijmegen division since 2018, which organises a course on lifestyle and also lobbies the Medicine degree programme to have the theme included in the curriculum.
Popular
That extracurricular course is full this year – due to the COVID-19 pandemic, there is room for a maximum of 70 students. Committee members Femke de Schutter (20) and Meike Kappen (22) are not surprised by the popularity. They see the enormous interest from students as proof that the Medicine degree programme in Nijmegen places too little focus on the subject.
‘We often hear how an unhealthy lifestyle leads to health problems, but we are given few tools with which to get to grips with that’, says De Schutter. ‘Even though these would help to tackle problems at the source, the cause, rather than combating symptoms.’ Kappen recalls lectures about the aftermath of cardiac arrest. ‘We were mainly given information about the medicines you prescribe the patient, such as beta blockers. But what you want is for people to start living a healthier life, so that the risk of a subsequent cardiac arrest is reduced.’
During the course, participants acquire more knowledge about the various facets of lifestyle such as nutrition, sleep, physical exercise, mental health and behavioural change. Speakers from the professional field share their expertise and engage in discussion with the students afterwards. The course ends with role play in which the participants act out a consultation and have to offer advice. If a patient with heart problems often flops onto the couch in front of the television, a short walk after dinner is a good idea. If a diabetes patient finds it difficult to cook healthy meals, they can consult a nutritionist.
In practice, this approach benefits everyone according to the organisation: patients feel better and pressure on the healthcare system is reduced. ‘By starting at an earlier age, you can often prevent diseases later in life’, says Kappen. She adds: ‘It’s important to me not to only treat patients at the end of the process, but to prevent symptoms from happening at all.’
Greater
Despite its success, the students hope to be able to stop the course at some point. But that will only be possible if there is sufficient focus in the standard degree programme for this subject. The Medicine degree programme took a first step towards this in 2019 with the introduction of a new elective about nutrition as medicine. But that doesn’t go far enough for De Schutter and Kappen. They want a greater focus on healthier living in all of the degree programme’s themes. ‘It takes a long time to change something that has been ingrained for so long, but we’re optimistic’, says De Schutter. She points to the new Raamplan Artsenopleiding (medical training framework plan) in which the theme is explicitly mentioned. ‘The degree programme is listening to our ideas more often. It’s a sign that there’s a lot of goodwill.’
The Student & Lifestyle lobby is in line with the broader view on lifestyle at hospitals and general practitioners, who are spending increasingly more time on nutrition and physical exercise. COVID-19 plays a major role in this: overweight patients end up in hospital with serious symptoms much more often than those who follow a healthy lifestyle. De Schutter therefore reaches the following clear conclusion: ‘The importance of a healthy lifestyle is actually greater than ever.’
Expert: too little focus on lifestyle up till now
Esther Aarts, researcher in Nutrition and Cognition at the Donders Institute, is extremely enthusiastic about Student & Lifestyle. ‘There has traditionally been little focus on a healthy lifestyle in the care sector. Thanks in part to initiatives like this one, we’re seeing that change. Doctors are beginning to address behavioural change more and more. It’s a question of what is necessary to have people live a healthy life at home.’
Although a change in attitude can be seen, Aarts warns that this turnaround will take effort. ‘The whole business model of the care sector is aimed at treatment rather than prevention. The health insurer often reimburses the cost of medicines, but not of a lifestyle coach. Even though medicines are often relatively more expensive.’
Aarts points to the ‘prevention paradox’: the prevention of health issues saves a lot of money but the effects at an individual level are not clearly visible. ‘Luckily, there is an increasing amount of long-term research which shows that prevention saves a lot of money. For example, we know that an unhealthy lifestyle in middle-aged people can lead to dementia later. Better prevention would result in savings of 2 billion euro a year with Alzheimer’s disease alone.’